For patients, surgery is simply the first step in a potentially daunting recovery process. Pain is almost synonymous with surgery, and pain is something patients prefer to soothe at home as opposed to inside a hospital. Indeed, it is now more common for shoulder surgery to happen in an outpatient center or ambulatory surgery center (ASC).
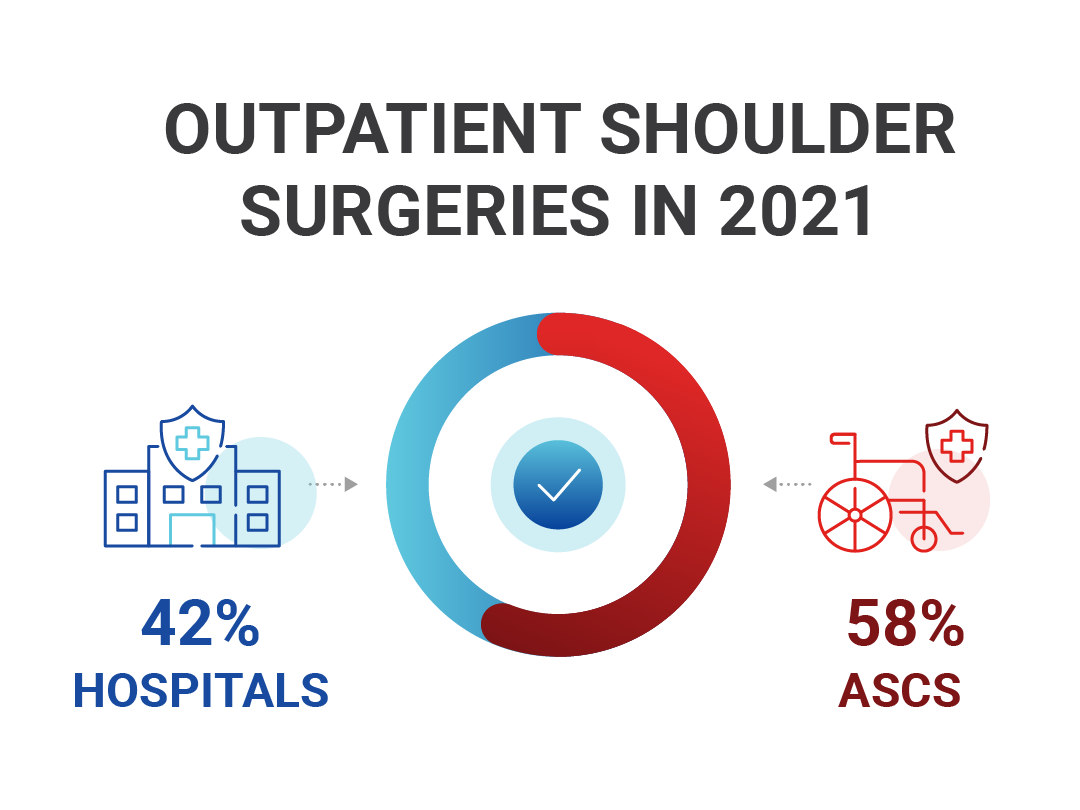
In 2021, Definitive Healthcare reported that more than 670K outpatient shoulder surgeries occurred in ASCs (approximately 58%) while only 390K shoulder surgeries took place in hospitals. More than ever before, patients overcoming surgery will be managing pain after being discharged from an ASC, and it can be difficult to manage a pain strategy without a healthcare professional nearby.
Pain management is key for ASCs as they take on more shoulder surgery cases each year. Whether it’s a total shoulder replacement, shoulder arthroscopy, or rotator cuff surgery, patients need options when it comes to at-home pain management.
There are several considerations when it comes to modern-day pain prevention.
The Different Types of Post-Op Pain

Post-surgery pain can be categorized as both chronic pain and acute pain.
- Chronic pain can last months to years post-surgery. It is persistent and varies in severity. Chronic pain is a burden and costly to treat. Currently, only one-third of surgery patients report developing chronic pain.
- Acute pain is something all patients will experience after surgery. This type of pain occurs immediately after the operation and can last longer than three months post-op as tissue heals. Don’t be fooled by the name, though; acute pain doesn’t mean small. It can be overwhelming for patients and drastically affects many aspects of day-to-day life.
Pain After Shoulder Surgery: the Problem for Patients
Pain is much more than an inevitable side effect, it impacts patients’ quality of life and can even delay the healing process. It’s no surprise that effective pain management is directly related to patient satisfaction.
- Some patients complain of difficulty sleeping due to medication lapsing and the inability to keep comfortable through the night. This problem creates a vicious cycle as the lack of sleep can delay healing. Sleep helps reduce cortisol levels, and high cortisol levels can delay growth hormones to rebuild tissues.
- With pain also comes limited mobility. After surgery, patients need to rest, but the pain can prevent a return to normalcy. Often, after surgery, a surgeon or physical therapist will prescribe exercises for recovery, but with intense acute pain, patients often avoid or prolong these important exercises.
- Pain is physical in nature, but it can also present mental health challenges such as depression and anxiety. Battling depression can make recovery feel impossible for many patients.
- In addition, not moving normally can cause blood clots to form in the deep veins, leading to deep vein thrombosis. Sometimes, pneumatic compression sleeves are prescribed post-surgery to help reduce the risks of blood clots.
Further reading: Learn how compression can help prevent the post-surgical complications of DVT.
Opioids and Pain Management
In the 1990s, opioids were introduced as a painkiller of choice that would revolutionize healthcare. These medications are very effective at reducing pain, but they can also come with significant side effects. A few of the minor side effects include dizziness, nausea, and constipation, but the real danger is the fact that opioids are highly addictive.
Opioid addiction is an ongoing public health crisis.
90% of surgeries still involve opioids in America, but the numbers simply don’t add up… 30% of patients with chronic pain misuse opioids, and up to 12% develop opioid use disorder.
In 2022 alone, nearly 80,000 drug overdose deaths involved opioids.
In 2016, the CDC published guidelines for pain management in hopes of moderating opioid usage, but there was some ambiguity in the initial draft.
Essentially, the “CDC’s Clinical Practice Guideline for Prescribing Opioids for Pain” outlines hard pain thresholds for medication and dosages. This document was intended to be a guide, yet many pharmaceutical shops turned the guidelines into policies that resulted in several misconceptions.
In 2022 the No Pain Act was passed, which is a step in the right direction.
The recommendations in the No Pain Act are easier to digest and more user-friendly. Instead of a “one-size-fits-all” approach, the new legislation allows physicians to make more informed decisions that are specialized for patients to manage pain.
The new guidelines also advocate for the usage of pain pumps. These devices allow the medicine to travel through a catheter, pushing intermittent delivery of medication. This helps patients manage breakthrough pain and is an opioid-free solution.
Opioid Sparing and Opioid-Free Approaches to Pain Management
There are three main categories for managing pain with limited or no opioids involved. These include non-pharmacological interventions, non-opioid analgesia, and interventional techniques.
1. Non-Pharmacological Interventions
Non-pharmacological interventions mean managing pain without any medications. This method often centers around a mind-over-matter approach of using the mind to focus on things other than pain.
Comfort therapy is a popular form of non-pharmacological intervention which can include exercise, companionship, and even heat or cold therapy. Physical therapy is also a pain intervention that can help ease symptoms.
2. Non-Opioid Analgesia
Analgesia means “the absence of pain.” While some opioids are considered analgesia medications, there are non-opioid analgesia medications available. Medications such as gabapentin and pregabalin are examples of non-opioid analgesia. These medications are typically prescribed for mild to moderate pain.
Antidepressants are also labeled as analgesia medications, but the non-opioid analgesia medications used for pain work by lowering neurotransmitter release.
3. Interventional Techniques
Interventional pain management is a multidisciplinary approach to pain management. This type of treatment can include injections, medial branch blocks, and also pain pumps. Interventional techniques are opioid-free and focus on managing breakthrough pain.
Pain pumps are surgically implanted, pumping a programmed amount of medication into a patient’s spinal cord. There are several different kinds of pain pumps.
Types of Pain Pumps
Pain pumps are an intrathecal drug delivery system that delivers medication straight to the source of the pain. But, not all pumps are equal.
This article explains how some pain pumps can relieve acute pain following shoulder surgery. Yet, other pain pumps are designed for patients experiencing chronic pain.
This is an opioid-sparing approach that delivers medication to the source. However, not everyone is a great candidate for a pain pump. Risks can involve infection after the implantation or even complications from anesthesia. Some patients also experience side effects such as headaches.
Below is a summary of the different types of pain pumps that are on the market, outlining guidelines for usage as well as associated risks.
| Pain Pumps | Summary | Advantages | Cons |
| Intrathecal Pain Pumps | Provides targeted pain relief, delivering medication in the spinal fluid. | Allows for better pain management and typically smaller doses of oral medication. | Small risk of infection after implanting the pain pump. |
| Patient-Controlled Analgesia (PCA) Pumps | Allows for patients to control how often they receive dosages. | Gives patients control of their pain management. | Risk of overdose if the patient administers the medicine too often. |
| Epidural Pumps | Pumps medicine directly into the spinal cord to help with pain management. Most often used for childbirth or post-surgery | Provides quality pain relief to the lower body. | Risks include headaches and low blood pressure. |
While there are some negative side effects to pain pumps, but these are mild compared to the risk of opioids. Overall these devices are a promising solution to reducing opioid use post-surgery.
What Does the Research Say About Pain Pumps?
What pain pump is the best option for your patients? Naturally, research varies depending on the type and quality of the pump used.
There are a variety of pain pumps on the market. The ambIT Pain Pump is an intrathecal pump developed by Avanos that can be used on pediatric and adult patients.
This is a great option for pain relief after shoulder surgery. Especially when it comes to reducing opioid prescriptions.
Research on the ambIT Pump
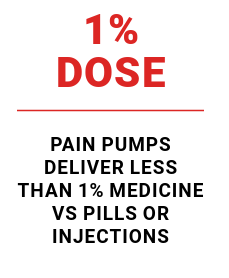
Intrathecal pumps such as the ambIT serve the purpose of managing breakthrough pain. Studies suggest that pain relief from a pump is accomplished at less than 1% dose of what is found in pills or injections.
The ambIT system also has a high patient satisfaction rate due to convenience and portability. With fewer side effects and enhanced recovery, pain pumps are a great solution for ASCs working to provide relief while keeping readmission rates low.
UCLA Implements the ambIT System
Hospitals and surgery centers across the US have successfully implemented the ambIT system. Some facilities have adopted ambIT as the first pain pump to use following surgery. Other facilities are using ambIT to upgrade their existing pain pump devices. These facilities are seeing benefits in patient satisfaction as well as reimbursement rates by utilizing ambIT.
In 2023, UCLA Santa Monica Hospital adopted the ambIT pain pump. Of course, adopting a new medical device in a major hospital system is no easy feat, and it took a year and a half to fully implement the device within the facility. However, the hard work and dedication to launching the product paid off.

Because UCLA Santa Monica is a hospital system, not an ASC, same-day discharge is not a guarantee. However, after implementing the ambIT pain management system, the hospital saw an increased amount of same-day discharges with post-operative patients. This has helped the hospital fight against the ongoing battle of bed shortages in hospitals as well as the opioid crisis.
Further reading: See a full report of UCLA’s success with the ambIT pain pump.
Anticipating Patient Questions about Pain Pumps
Because many patients have not heard of pain pumps, healthcare providers must be prepared to address skepticism and basic questions from patients.
Frequently asked questions include:
Are pain pumps reimbursable by insurance?
Yes, the ambIT pain pump is typically reimbursable by insurance as it qualifies as durable medical equipment. However, reimbursement rates vary from patient to patient as well as state to state.
Some risk factors that are considered when it comes to insurance coverage and reimbursements include:
- Current or former opioid use
- Family or personal history of substance abuse
- The patient wants to avoid opioid drugs
- Current smoker
- History of anxiety, insomnia, or seizures
How does the pain pump work?
When a patient is prescribed the ambIT pain pump, a catheter that is connected to the tubing attaches the infusion pump to the patient.
The catheter is held in place with adhesive tape on the patient’s back. The pump allows medication to be distributed to the body automatically.
Can I move when I’m using the pain pump?
Yes, one of the advantages of the ambIT pain pump is that patients can carry the pump in a bag. They have the ability to move around and continue daily tasks. However, patients should keep in mind that it should not be used while taking a shower.
This enhanced mobility can help patients recover faster. Movement will help restore blood flow back to its natural state, helping prevent DVTs and other postoperative complications.
How do I remove the pain pump when I need to?
Most pain pumps are prescribed for five days postoperatively unless your provider says otherwise. Afterward, patients can easily remove their ambIT pain pump at home . To remove, start by carefully removing the medical tape holding the catheter and then carefully pull out the catheter. It is a good idea to place an adhesive bandage over the area where the catheter was located.
Implementing Pain Pumps in Your Surgery Center
Presenting the device to surgeons, surgery center administrators, and other decision-makers can be a hard push, but Compression Solutions has worked with numerous ASCs to make the process as seamless as possible.
Leading up to launching a system, Compression Solutions and Avanos will have a representative inside your facility to answer questions about using the device and medical billing. After training, there are still plenty of resources for your surgery center to experience a seamless transition to using the ambIT.
Recently, Compression Solutions worked with University Center for Ambulatory Surgery (UCAS) to implement the ambIT program. This particular surgery center wasn’t a stranger to pain pumps. They had been utilizing a different pain management system. But, decided to switch to ambIT for updated technology and unique medical billing services provided by Compression Solutions.

“The biggest hurdle to overcome [when launching a new program] is time you need to make the change,” says Susan Gurwitz, administrator at UCAS. “Everyone gets so caught up in the day-to-day with the attitude of ‘if it’s not broken don’t fix it.’ That mindset needs to change.”
“It’s something the doctors believe in. They believe in this method and product for patients. It’s savings for the center and a better option for patients” – Susan Gurwitz, UCAS
Before prescribing the new device. The staff at UCAS participated in training on the new devices. After learning about the new program and feeling more confident, the staff saw the upsides of ambIT.
UCAS officially launched the ambIT program which led to a $34,000 savings in just the first six months of this program.
Case study: Read a full synopsis of UCAS’s implementation of the ambIT pain pump.
Access Our New Ebook on Effective Pain Management
Discussing modern pain management should not be a pain. All clinicians know that pain is the most common complaint after surgery. They also know about the dangers of opioids.
Fill out the form below to access our free e-book that dives into effective pain management for the modern surgery center.
Download this free e-book to learn more about:
- Facts about the current opioid crisis
- Deeper insight into pain management
- The needs of ASCs when it comes to patient care
- Regulatory changes: what you need to know
- Opioid-sparing approaches
- Cost Efficiencies and Long-Term Savings
- Reimbursement information for pain pumps
E-Book Signup: Effective pain management after ASC surgery
Enter your information to download your free e-book discussing how ASCs can help mitigate the opioid crisis with new pain management solutions.
Get ambIT for Your Facility
Equip your hospital or surgery center with ambIT pain pump devices, including convenient medical billing and customer support when you order through Compression Solutions.
