ASC costs rising, staff shortages, and reimbursement woes plague ASCs across the country. What’s the solution?
Ambulatory surgery centers (ASCs) are getting more popular every day. Patients prefer the value proposition — value-based care for successful elective procedures without the frills.
But to keep the lights on, the low-margin world of ASCs needs to:
- Lower the costs of doing business and remove inefficiencies
- Keep recruitment costs low and retain staff
- Shorten medical billing and revenue cycles
Unfortunately, it is getting harder and harder for ASCs to do so.
Operating costs are rising. The entire healthcare industry is struggling to find qualified candidates and retain staff, and the maze of revenue cycles makes reimbursement cycles longer.
Why are ASC costs rising?
A 2022 study across 380 ASCs showed that operating expenses were a staggering 76.8% of net operating revenue — a financial tightrope. Also, the median operating costs across all facilities studied were $6.9 million. This amount is quite high, considering the lower revenue compared to hospitals.
The main reasons for these escalating costs are:
Higher supply costs
ASCs require a range of medical supplies and consumables, including surgical instruments, gowns, gloves, drapes, and medications. The cost of these supplies has increased significantly in recent years. To get better rates, suppliers demand larger orders. While this may be possible for a few larger ASCs, most may not be able to buy in bulk to receive better pricing.
Buying in bulk has its disadvantages too. While it is a standard way to keep costs low, ASCs must manage bigger inventories. This ‘solution’ brings a slew of new challenges and costs.
Apart from essential medical consumables, ASCs must invest in medical equipment and technology to provide high-quality care to their patients. With technological advances, equipment becomes more sophisticated and more expensive.
Staff shortages and hiring costs
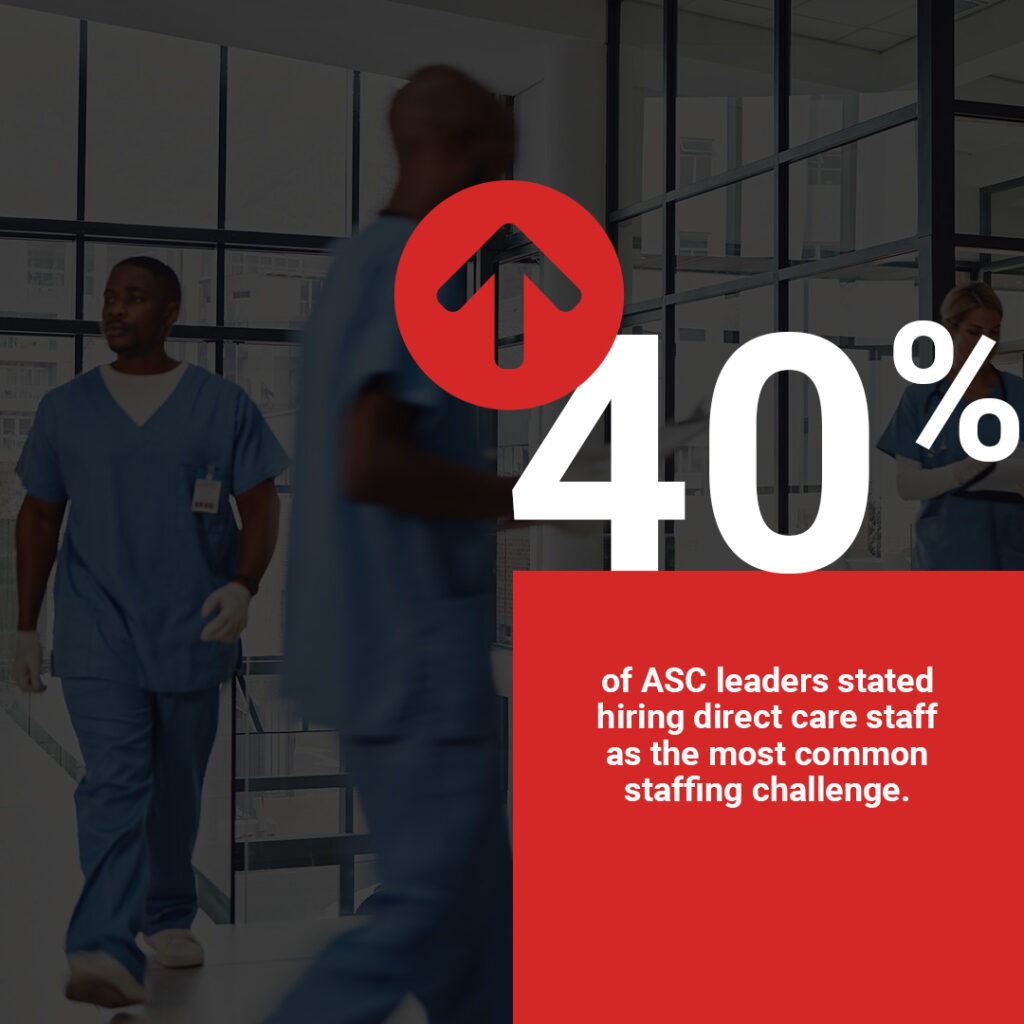
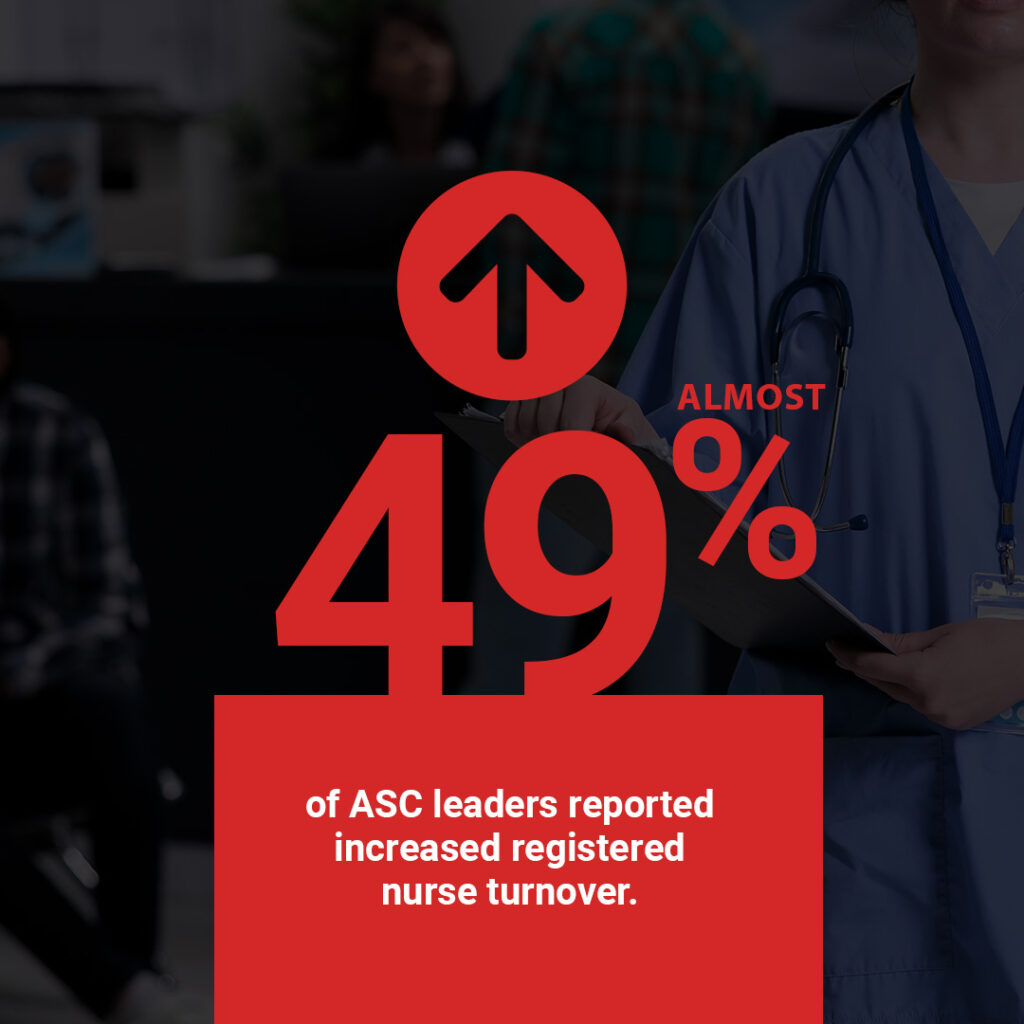
In an ASC benchmarking study, 40% of ASC leaders stated that hiring more direct care staff was the most common staffing challenge. Almost 49% of ASC leaders reported increased registered nurse turnover. Fighting intense competition
ASCs require a team of highly skilled medical professionals to provide care to their patients. But with more centers sprouting nationwide, there is intense competition for qualified healthcare professionals and staff. This makes it harder to retain existing employees.
ASCs have to spend more to recruit and retain the right teams and continue to offer quality care to their patients. Currently, ASCs spend almost 21.3% of net revenue on employee salaries and wages. Risk of burnout
Plus, ASCs run a tight ship with lean teams. While this is great for the bottom line and keeps surgery centers agile, it can be challenging as patient volumes continue to rise. With a shortage of skilled professionals on board, burnout is a risk.
A revolving door of qualified professionals is difficult for any industry to manage. But there are stronger consequences in the complex and highly regulated world of healthcare. A high turnover affects employee engagement and, ultimately, patient engagement and satisfaction. Skilling and resource challenges
A significant pressure on ASCs (that hospitals do not have) is that because of same-day discharges, the staff have a limited window to collect, confirm, and edit or correct patient data required for reimbursement.
For example, ASCs have a tightly packed OR schedule. Surgeons do not have enough time for dictation and proofreading transcribed reports, and the staff does not have enough time to fill in details or find the right codes. Even if a third-party handles revenue cycle paperwork, ASCs staff still have the burden of providing details about patients and their procedures.
Following up with patients after each procedure takes time and effort and lengthens the reimbursement cycle. When your staff is stretched thin, there is not enough time or resources to train new employees and streamline the revenue cycle.
Costs rise, reimbursements drop — what’s an ASC to do?
ASCs are the new normal for successful elective procedures like primary hip and knee replacements. Patients and payors like them for their value-based care approach — quality care without a premium price tag attached.
However, running an ASC in the face of rising operational costs, staff shortages, and extended revenue cycles is no easy feat. As costs rise, reimbursements continue to drop. How do ASCs thrive in such an environment?
Automation platforms designed for ASCs are an excellent way to:
- Relieve the burden on lean teams that are stretched thin
- Reduce onboarding and training costs for new staff members
- Empower highly efficient OR teams with faster turnaround, less time spent on record-keeping and keeping medical staff out of accounts receivable
- Minimize the risk of coding and other paperwork-related errors that extend the reimbursement cycle.
Enable same-day billing for your ASC with Pro-Mapp
Pro-Mapp is a unique platform built to streamline ASCs. With Pro-Mapp, you get coded and signed operative reports as soon as a procedure is over (no dictation needed from surgeons). This way, you can bill on the same day a procedure is completed.
The Pro-Mapp team also customizes the platform for your ASCs needs, which saves time and resources, and helps you get reimbursed faster.
