Most healthcare providers can agree that accurate patient data is essential for providing high-quality healthcare services.
Yet only 38% of healthcare providers are “fairly confident” their patient data is accurate, according to a 2021 TransUnion Survey.
Missing or inaccurate information about insurance, referrals, and patient demographics can add significant delays to the billing, claims, and overall revenue management cycle.
When they compound, these errors come at a huge cost for surgery centers.
The Cost of Data Entry Errors in Electronic Medical Errors
Patient data errors caused by data entry or other human and technical factors can lead to a whole host of problems such as:
- Incomplete data to evaluate patient-reported outcomes measures (PROMs)
- Delayed research when having to resubmit IRB paperwork
- Higher costs and wasted time for staff
- Higher rejection rates from payers
- Delayed claims submissions
Even before the pandemic, healthcare providers have felt the burden of demanding workloads, with one in three physicians experiencing burnout at any given time.
Delays caused by medical errors strain healthcare personnel further.
ASCs Face Unique Challenges to Avoiding Medical Errors in Data
Ambulatory Surgery Centers face particular hurdles when collecting patient data.
With cost-effective prices for routine surgeries, ASCs are transforming how healthcare works. byAs a result, demand for outpatient care is growing at a faster rate than inpatient care. The only way to satisfy demand and manage costs is to run hyper-streamlined surgery centers.
However, compared to hospitals, ASCs face several unique issues when it comes to collecting patient data without delays or errors.
Challenge #1. Limited In-Person Time With Patients
An ASC’s biggest strength is also a disadvantage when it comes to patient data collection.
Patients prefer ASCs because they can receive outpatient procedures without being admitted into a hospital. This way, they save costs and recover in the comfort of their own homes. The issue with this care model is that since patients are discharged the same day, tASC staff have little time to verify or validate information with a patient directly.
To overcome this limitation, staff members have to call or message ahead to gather patient demographics, insurance information, and more. For ASCs already struggling with staff shortages and limited resources, it can be hard to track patients down and ensure all information is complete and accurate before a procedure.
Challenge #2. Timing is Hard to Master
As the number of ASCs increases, so does the competition. And with this growing competition, it’s not uncommon for patients to shop around before making a choice. Your patients may reschedule or cancel surgery altogether if other priorities get in the way of their elective procedures.
Collecting data too soon may be a wasted effort — a patient may not commit to surgery at your center. But waiting until it’s too late may inconvenience the patient, result in missing information, and increase the chances of claims denials.
To make things worse, technology that is supposed to help with patient communication is often woefully inadequate. EMRs are notoriously difficult to use, and the vast majority of patient technology platforms are clunky and awkward. It’s also easy for patients to miss emails from their healthcare provider, since most technology software do not share the surgery center’s branding.
Challenge #3. Difficulty with Post-Surgery Data Reconciliation
Another reason why claims may get delayed or even denied is the details of a procedure differing from the approved payer package for that surgery.
ASCs do collect each patient’s insurance information before surgery, but they cannot complete the entire process beforehand. Sometimes, surgeons may deviate from a surgical plan based on intraoperative assessment of bone and soft tissue quality, and modifiers like obesity, comorbidities, and more. Correlating insurance information can be difficult post-surgery when different teams and software platforms are involved.
Often, staff may have to keep following up with patients and their insurance companies (or Medicare) to validate and verify critical data holding up payments. This can be a huge drain on resources in ASCs, where every penny counts. Having to contact patients multiple times after surgery can also risk antagonizing them, resulting in lower satisfaction levels. When patients disengage, this can adversely affect PROM data collection as well.
How ASCs Can Get Patient Data Right the First Time
So now that we’ve explored the challenges and cost of errors in medical data, how can ASCs avoid these errors altogether? Let’s explore a few key solutions.
Solution #1. Collect Patient Details During Registration.
The first solution is to collect data, including patient demographics, in the waiting room just before surgery. At this stage, patient engagement is high. They are more willing to give you the information you need. Using this time may also benefit your staff as the data collection process can be a welcome distraction for patients worrying about their upcoming surgeries.
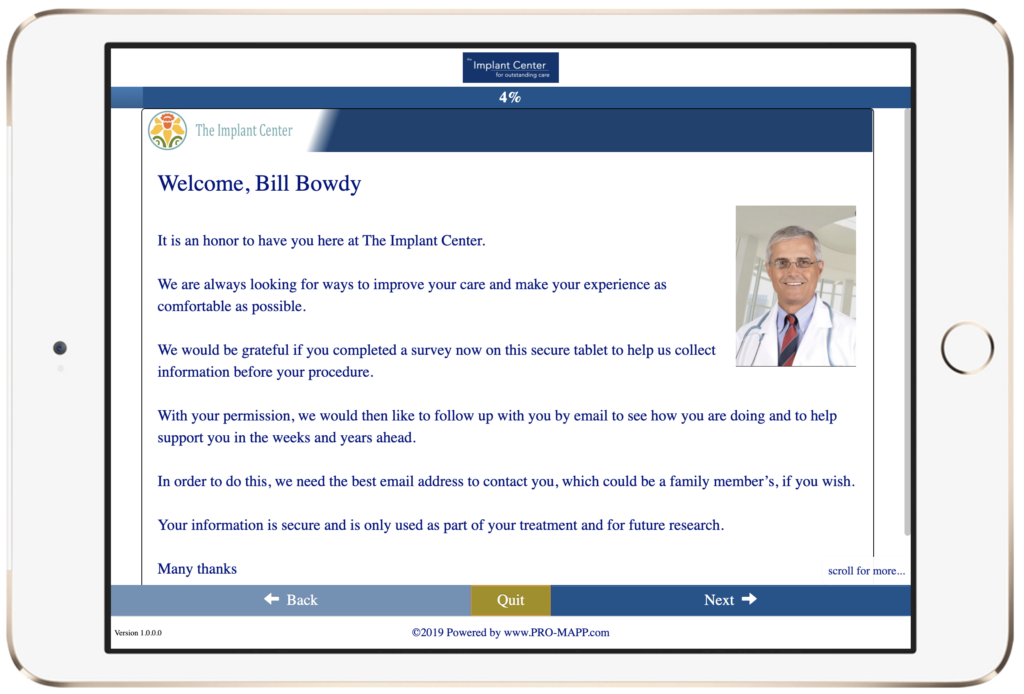
If you use a digital solution like PRO-MAPP that is designed to improve efficiency in ASCs, you can also scan insurance documents and any other vital information at this stage and store it all in one handy location.
Solution #2. Recognize That EMRs Don’t Have All the Answers
Solution #2. Recognize That EMRs Don’t Have All the Answers
Unfortunately, many software solutions like EMRs and EHRs were made to store information, but not help capture it. They can be difficult to use and often don’t offer streamlined workflows. To make data collection simpler for staff and patients, many ASCs have resigned themselves to using paper forms. But this doubles the work — all data then has to be manually entered into an EMR. This extra step results in a greater likelihood of errors.
A user-friendly digital platform designed with ASCs in mind can be a gamechanger.
Accessible participation from the patient can help decrease data errors. With some softwares, admin staff can hand a tablet over to your patient while they wait for surgery. With integrations to EMRs and EHRs, this creates a streamlined, hassle-free, automatic data transfer.
Solution #3 Add a Personal Touch to Improve Response Rates
People connect with other people — not through impersonal forms or emails. Infuse all your patient communication with your personal touch to engage your patients through their surgery journey. Platforms like PRO-MAPP can help you boost engagement with enhanced digital communication.
With PRO-MAPP, you can personalize all your communication with your surgery center’s branding, a friendly photo of their physician, and much more. Your center and surgeons can engage with each patient whether they’re in your waiting room or at home, and patients will be more likely to respond to your communications.
Eliminate Data Entry Errors in Electronic Medical Records The First Time
ASCs that are willing to try new tactics and tools to get their patient data right have a huge opportunity on their hands.
With software like PRO-MAPP and tactics like personalized communications and data upon patient registration, ASCs can achieve greater efficiency, profitability, and patient satisfaction.
If you’re interested in learning more about how PRO-MAPP can benefit your ASC, we encourage you to contact Compression Solutions today.
And, if you’re ready to take your billing processes to the next level and achieve same-day medical billing, be sure to download our free ebook on the topic.
With the right tools and strategies in place, your ASC can thrive in the digital age and you can provide the highest quality care to your patients.
