Resources
Your hub for medical device news, tips and tricks for running a surgery center, and resources for reps.
For the latest information, sign up for our newsletter.
Featured Articles
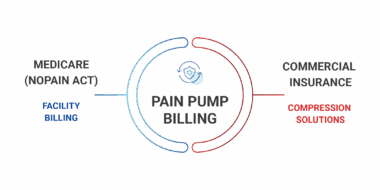
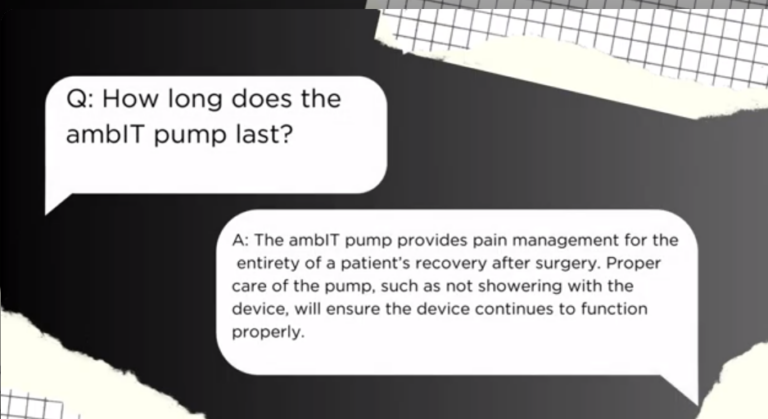
NOPAIN Act Billing Opportunities for Pain Pumps
The NOPAIN Act officially went into effect in January 2025, and it’s already changing the landscape of post-operative care…
Pain Management Billing for ASCs: Tips to Avoid Common Pitfalls
Pain management after surgery can be, well, a “pain.” Everyone in a surgery center environment has to work in…
Ebooks
Grow with Compression Solutions
Equip your hospital or surgery center with medical devices, software and billing services from Compression Solutions