Medical billing can be cumbersome, confusing, and time-consuming. This article provides a guide to help surgery center administrators and other healthcare providers better understand and communicate the medical billing process.
The Financial Impact of Medical Billing
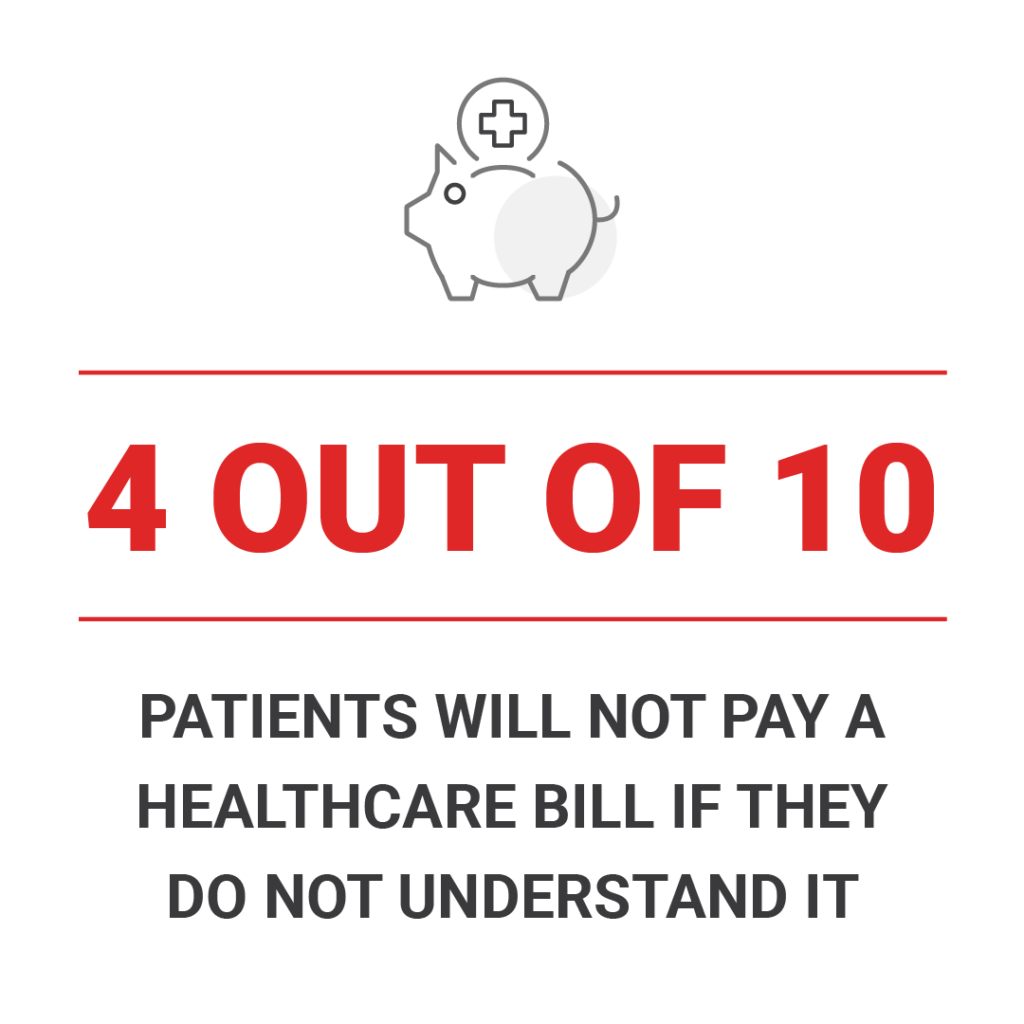
Issues with medical billing costs healthcare providers millions every year. In fact, 4 out of 10 consumers will not pay a healthcare bill if they do not fully understand it.
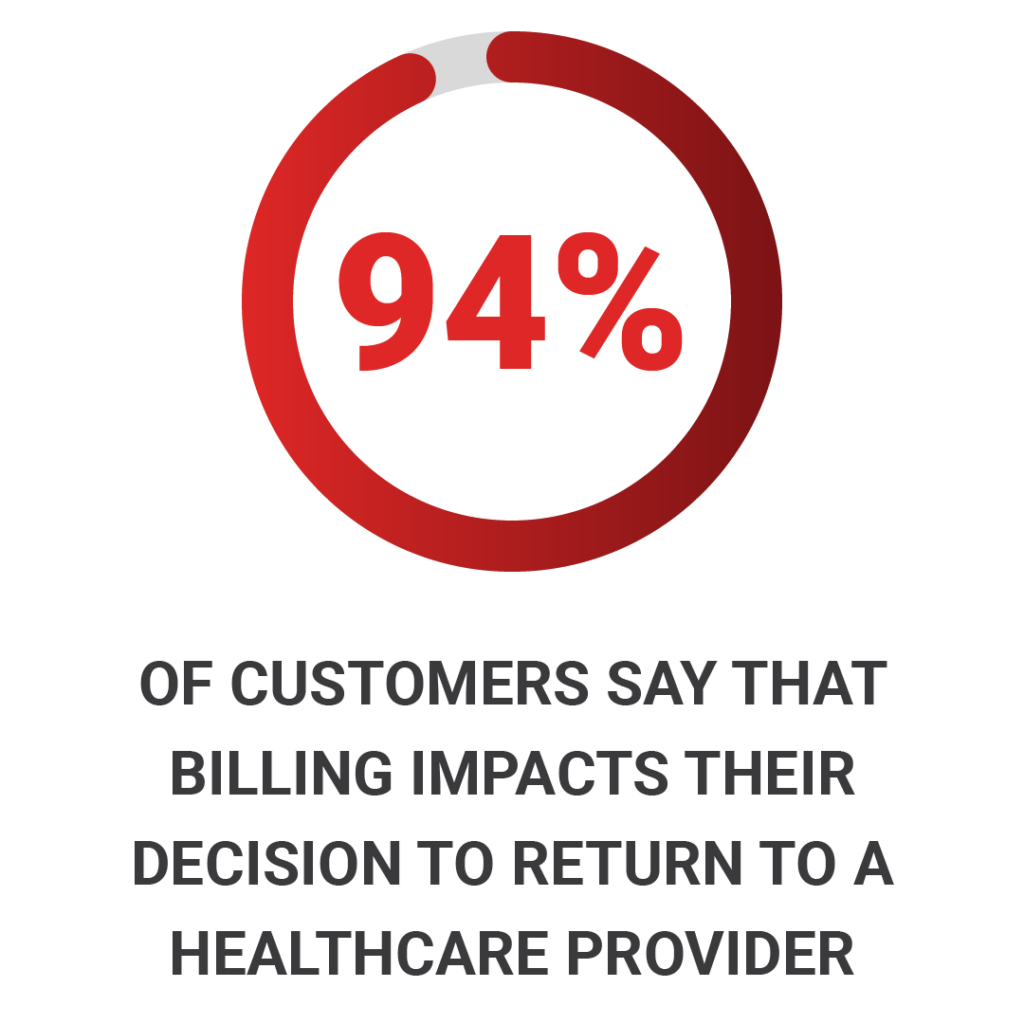
Billing is such a sensitive subject for patients that it can drive future healthcare decisions. According to a Healthcare Finance Study, 94% of customers say that billing is an important factor when choosing whether to return to a provider. Nearly 38% of customers have switched medical providers due to a negative billing experience.
Medical billing aids the sustainability of healthcare practice. It helps facilities receive payment, but it also allows patients to receive products or services that assistance before, during, and after surgery.
Key Steps in the Medical Billing Process
Typically, there are four key steps when it comes to medical billing.
Step 1: Patient Check-in and Verification
Patients expect to be greeted with a mountain of paperwork when they visit the doctor. Some forms are for the provider, but others are for the medical billing company. Streamlining this step can improve patient experience and reduce time between service and billing.
Further reading: Ways facilities can reduce errors during patient check-in.
Step 2: Medical Coding of Diagnosis and Procedures
Coding is a cumbersome part of the billing process when a medical biller will read through paperwork and match ICD10 codes to procedures. It is vitally important that all patient information is correct to obtain accurate coding for reimbursement.
Sometimes durable medical equipment is used within the surgical process. But, who pays for the extra equipment: the facility or patient? Insurance often covers products to aid in the health and well-being of the patient, and therefore, a billing team will usually work with insurance on reimbursement.
Step 3: Charge Entry and Claims Submission:
After coding takes place, the documents are typically uploaded into a medical billing system before the claim will be billed. If the claim is sent via paper instead of a digital format, it will be mailed out the following business day.
Step 4: Payment Posting and Follow-up
After the payment is posted, the billing company will follow up with the insurance company to make sure all patient information is correct.
The Importance of Medical Billing in Healthcare and ASCs
At their core, medical billing departments help patients get the most out of their insurance coverage, and they help healthcare providers ensure financial health.
Facilitating Patient Care
Effective medical billing should not directly involve the patient until an accurate and informative bill is available. It is also helpful if there is someone the patient can call with questions outside of their medical provider.
Ensuring the Financial Health of Healthcare Providers
Effective medical billing helps surgery centers prescribe products that they could not necessarily financially cover for patients. It can also decrease administrative burden and reduce time between service and billing.
Interested in working with a seasoned billing team for durable medical equipment? Here is the Compression Solutions process.
Navigating Challenges in the Medical Billing Process
The billing process may sound straightforward, but sometimes insurance companies will deny or appeal a claim. Other times, patients will not fully understand why they are billed.
Any issues with medical billing stand to delay time to reimbursement and negatively impact the patient experience.
Dealing with Insurance Denials and Appeals
Denials and appeals typically mean the insurance company has seen errors or missing information in a patient’s medical records—yet another reason why complete paperwork is important. When this happens, the billing company will file an appeal and go back to the facility for more information.
Sometimes insurance coverage is denied because the insurer has deemed a product or service not medically necessary or simply not covered.
When paperwork goes back and forth between surgery centers and billing companies, it is time-consuming and delays the entire billing process.
Managing Patient Billing Questions and Concerns
Patients represent another potential road block in the billing process. Confusion can lead to delayed or missed payments, so clear communication is critical.
Oftentimes, a patient is at home recovering from surgery when they receive a mystery bill in the mail from a company they have never heard of. Facilities need to explain what DME patients will be sent home with following surgery and note any third-party providers that may be sending a bill.
Following a surgery, responsive customer service can help alleviate concerns and expedite the process—without further burdening the healthcare provider.
Mastering the Medical Billing Process
Medical billing can be time-consuming and cumbersome, but working with a good billing partner can help the process run smoothly.
Correct patient information is key to a smooth billing process, and, proper communication with patients will help alleviate communication gaps.
